-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
January 2024
Oesophagectomy specimen of a 74-year-old female.
Diagnosis
IgG4-related oesophagitis.
Comment
Oesophagectomy was performed in a 74-year-old female with long standing history of severe inflammation causing dysphagia and reflux symptoms non-responsive to treatment with proton pump inhibitors. A series of biopsies had not rendered a definitive preoperative diagnosis.
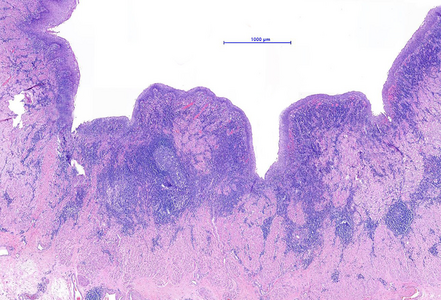
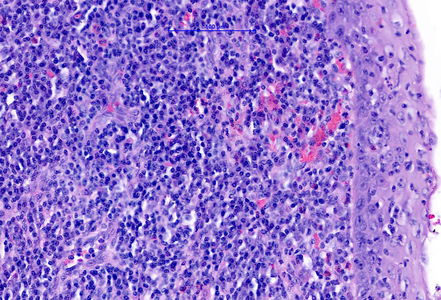
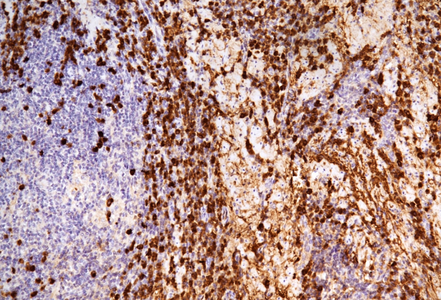
The microscopic examination of the resection specimen revealed diffuse lymphoplasmacytic infiltration throughout the oesophageal wall, with multiple lymphoid follicles and accentuation within the inner half (Panel A). On high magnification, diffuse infiltration of the overlying squamous epithelium by lymphocytes („lymphocytic oesophagitis pattern of injury”) and occasional plasma cells was observed (Panel B). The plasma cells were strongly positive for IgG and IgG4 (Panels C-D).
IgG4-related disease represents a systemic autoimmune disorder that is characterized by elevated serum IgG4 levels and tissue infiltration by IgG4 positive plasma cells. The infiltration causes fibro-inflammatory changes within various organs, including the pancreato-biliary tract, the retroperitoneum, the salivary glands, and the head and neck region. Upper gastrointestinal tract involvement is rare.
Clinically, manifestation of oesophageal stenosis is possible, with consequential therapy-resistant dysphagia, odynophagia, acid reflux, epigastric pain, and weight loss. Endoscopic examination may describe ulcers, strictures, and a potential submucosal tumour, especially in even rarer, localised cases. The final diagnosis is based on the examination of autoimmune panel and serum IgG4 test, and/or histology. Patients are primarily treated with corticosteroids, and later on with immunomodulators. Due to the above mentioned possibility of stricture formation, surgical therapy has to be considered, as well, including dilation or resection of the oesophagus.
Morphologically, IgG4 positive, dense, lymphoplasmacytic infiltrate is visible, with >10 plasma cells per high-power field. The elevated ratio of IgG4/IgG (>40%) is observed, as well. Furthermore, storiform fibrosis, and obliterative phlebitis may be seen, although these features may not be present on small biopsy specimens. At least 2 of the above mentioned criteria results in the definitive diagnosis of IgG4-related disease. Differential diagnosis on small biopsies includes lymphocytic oesophagitis.
For further reading
- Obiorah I, Hussain A, Palese C, et al. IgG4-related disease involving the esophagus: a clinicopathological study. Dis Esophagus. 2017;30:1-7.
- Padniewski JJ, Thottam G, Nasr R. IgG4 sclerosing disease of the esophagus: a case-based review. Rheumatol Int. 2020;40:1733-1737.
- Correia C, Moreira H, Almedia N, et al. IgG4-related esophageal disease presenting as esophagitis with chronic strictures. GE Port J Gastroenterol. 2021;30:68-70.
- Ekinci N, Kocabey DU, Gun E, et al. Giant IgG4-related pseudotumor of the esophagus resected with endoscopic submucosal dissection: A case report and review of the literature. Turk Patoloji Derg. 2021;37:258-263.
- Enea D, Camus M, Fléjou JF. An unexpected esophageal inflammatory lesion. Gastroenterology. 2021;161:e35-e38.
- Zhang B, Lai Y, Xu Y, Wang J, et al. IgG4-related oesophageal disease with Cytomegalovirus infection: A case report. J Pers Med. 2023;13:493.
Presented by
Dr. Anita Sejben, Szeged, Hungary, Dr. Cord Langner, Graz, Austria.