-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
September 2024
Colon biopsies from a 66-year-old male with chronic diarrhoea.
Diagnosis
Collagenous colitis with giant cells.
Comment
A 66-year-old male patient presented with chronic watery diarrhoea and faecal incontinence. Colonoscopy showed nearly normal colon mucosa lacking obvious pathological changes; step biopsies were taken.
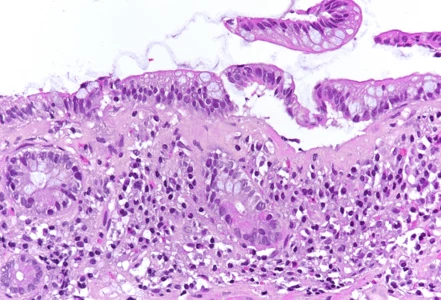
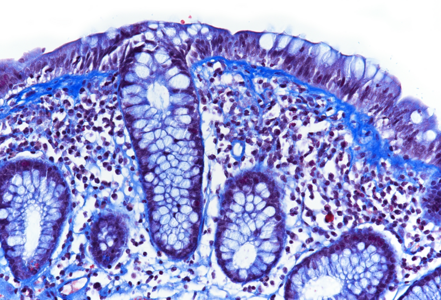
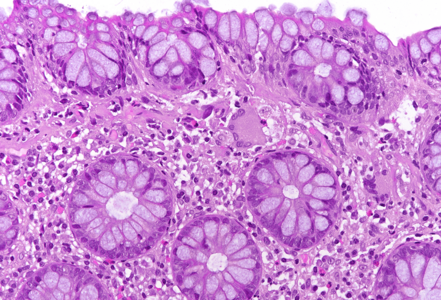
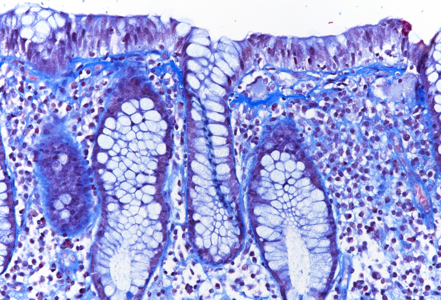
Histologic examination showed irregularly flattened large-bowel mucosa with diffusely increased inflammation in the lamina propria, the inflammatory infiltrate consisting of plasma cells, lymphocytes and eosinophils. In all biopsies, a prominent, irregularly thickened (> 10 µm) collagen band was observed under the surface epithelium (Panel A), which could be highlighted by modified trichrome staining (CAB; Panel B). The surface epithelium was detached and showed degenerative changes. No crypt architectural distortion or metaplastic changes were observed, and no signs of active inflammation were present. Interestingly, several multinucleated giant cells were seen in the lamina propria close to the thickened subepithelial collagen band (Panels C-D).
Collagenous colitis is a histological subtype of microscopic colitis, an inflammatory condition of the colon that causes chronic or recurrent watery, non-bloody diarrhoea. Microscopic colitis usually shows no or minimal mucosal changes on endoscopy but demonstrates typical histological changes. Collagenous colitis is characterized by thickening of the subepithelial collagen band (> 10 µm). The key feature of other histological subtype, lymphocytic colitis, is an increased number of surface intraepithelial lymphocytes (> 20 per 100 epithelial cells).
Giant cells have been described in both collagenous and lymphocytic colitis and they appear to be of histiocytic origin (CD68+). Their role in pathogenesis and the reason for their appearance remain unclear. Collagenous colitis with giant cells as well as lymphocytic colitis with giant cells are considered as variant forms of microscopic colitis without clinical significance.
For further reading
- Langner C, Aust D, Ensari A, Villanacci V, Becheanu G, Miehlke S, Geboes K & Münch A; on behalf of the Working Group of Digestive Diseases of the European Society of Pathology (ESP) and the European Microscopic Colitis Group (EMCG) (2015) Histopathology 66, 658–663. Histology of microscopic colitis—review with a practical approach for pathologists
- Freeman HJ, Nimmo M. Carpet-like polypoid lesion in collagenous colitis with mucosal giant cells. Can J Gastroenterol. 2011 Apr;25(4):187-8.
- Libbrecht L, Croes R, Ectors N, Staels F, Geboes K. Microscopic colitis with giant cells. Histopathology. 2002 Apr;40(4):335-8.
- Sandmeier D, Bouzourene H. Microscopic colitis with giant cells: a rare new histopathologic subtype? Int J Surg Pathol. 2004 Jan;12(1):45-8.
Presented by
Dr. Johanna Köhler, Linköping, Sweden and Dr. Cord Langner, Graz, Austria.