-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
October 2024
Colon biopsies from a 73-year-old female with haematochezia.
Diagnosis
Intestinal vasculitis with granulomatosis.
Comment
A 73-year-old woman with a medical history of lichen planus presented with abdominal pain and haematochezia. Colonoscopy was performed and demonstrated severe segmental ulcerative colitis in the transverse and sigmoid colon while no signs of inflammation were observed in the terminal ileum and the other parts of the colon and rectum. In addition, an ulcerated perianal skin lesion was noted.
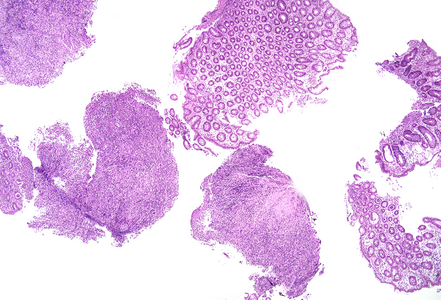
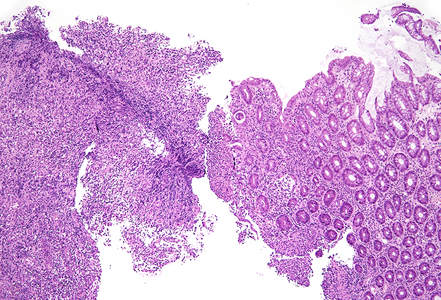
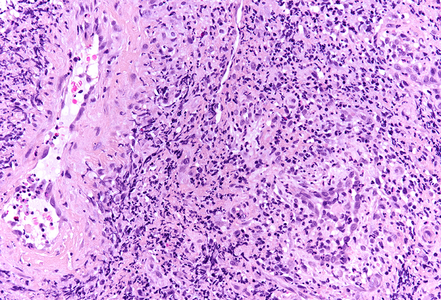
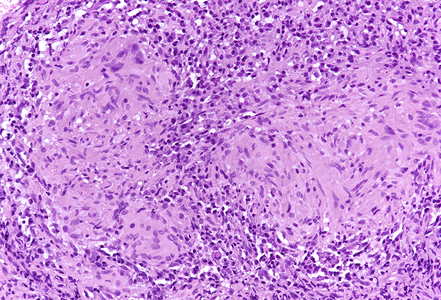
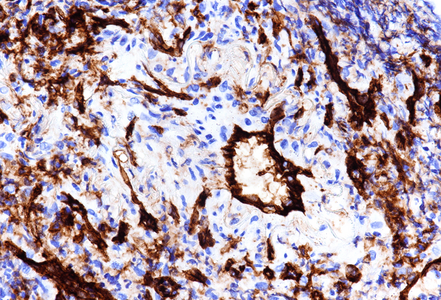
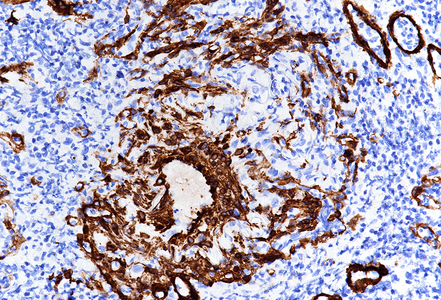
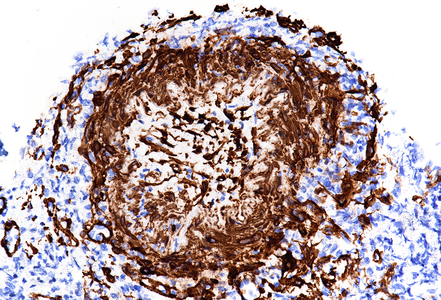
Microscopical examination showed unremarkable mucosa from the terminal ileum and most of the colonic biopsies. In biopsies from the transverse and sigmoid colon, fragments of only slightly altered colon mucosa were admixed with heavily inflamed and deeply ulcerated tissue, some biopsies consisted mainly of granulation tissue (Panel A). The preserved fragments of colon mucosa showed foci of acute inflammation with aphthous erosions, fissuring ulceration and occasional crypt abscesses. Crypt withering bordered mucosal defects (Panel B). Reactive and regenerative epithelial changes were noted in some of the biopsies, and small areas showed irregular crypts and pseudo-villous change, but no true architectural distortion or metaplastic change were observed. In the submucosa, small to medium-sized venous and arterial vessels showed marked infiltration of lymphocytes and neutrophilic granulocytes accompanied by wall thickening, focal fibrin deposition within the vascular wall and reactive endothelial cell changes, consistent with vasculitis (Panel C). Non-necrotic epithelioid cell granulomas were seen in association with the inflamed blood vessels (Panel D). Immunostaining for CD 31 (Panels E-F) and for smooth muscle actin (Panel G) highlighted the inflamed and partly obliterated vessels. No giant cells and no foreign material were detected. Few eosinophilic granulocytes were present within the surrounding inflammatory infiltrate.
Intestinal vasculitis with granulomatosis is a rare finding in intestinal biopsies and differential diagnosis includes granulomatosis with polyangiitis (formerly known as Wegener’s granulomatosis), Behcet’s disease and Crohn’s disease. Intestinal involvement by microscopic polyangiitis with granulomatosis is reported in up to 11% of cases and any part of the small and large intestine can be affected. Intestinal involvement in Behcet’s disease is seen in up to 60% of cases and the ileocecal valve is the most involved site. In rare cases of microscopic polyangiitis with granulomatosis and Behcet’s disease, gastrointestinal manifestation is the first and leading sign of disease. Symptoms resemble those of chronic or acute bowel ischemia and in severe cases, bowel wall necrosis and perforation can occur. Histopathological examination can be essential in making the diagnosis but is not always contributary since inflamed blood vessels and granulomas might not be represented in superficial biopsies. The overlying mucosa often shows nonspecific inflammation, ulceration and ischemic changes. Since a considerable histomorphological overlap between gastrointestinal involvement by vasculitis and Crohn’s disease exists, correlation of the histopathological changes with the patient’s history, clinical (extraintestinal) findings and laboratory test results is needed.
The patient in our case had a medical history of lichen planus, but no inflammatory bowel disease or systemic vasculitis was known. Besides affecting the skin, Lichen planus is known to involve the oral mucosa, anogenital region and rarely even laryngeal and oesophageal mucosa. No intestinal involvement has been described so far and the histological features in obtained colon biopsies were not suggestive for a lichen planus-related intestinal lesion. Biopsies from the macroscopically described perianal skin lesion showed unspecific dermal inflammation without evidence of vasculitis, granuloma or lichenoid dermatosis. The case was eventually signed out with a descriptive diagnosis of ‘colitis due to intestinal vasculitis with granulomatosis’ together with a comment that clinical correlation, further investigation and laboratory tests might be needed. Complementary testing for autoantibodies showed elevation of unspecific antinuclear antibodies (ANA), but anti-neutrophil cytoplasmatic antibodies (ANCA) were not detected. Treatment with corticosteroids and mesalamine led to complete improvement of symptoms but unfortunately, the final diagnosis remained unclear.
For further reading
- Storesund B, Gran JT, Koldingsnes W. Severe intestinal involvement in Wegener's granulomatosis: report of two cases and review of the literature. Br J Rheumatol. 1998; 37: 387-90.
- Naganuma M, Iwao Y, Kashiwagi K, Funakoshi S, Ishii H, Hibi T. A case of Behçet's disease accompanied by colitis with longitudinal ulcers and granuloma. J Gastroenterol Hepatol. 2002; 17: 105-8.
- Brown I, Kumarasinghe MP. Granulomas in the gastrointestinal tract: deciphering the Pandora’s box. Virchows Arch 2018; 472: 3–14.
- Lu CY, Hsieh MS, Wei KC, Ezmerli M, Kuo CH, Chen W. Gastrointestinal involvement of primary skin diseases. J Eur Acad Dermatol Venereol. 2020; 34: 2766-74.
- Feakins R, Torres J, Borralho-Nunes P, Burisch J, Cúrdia Gonçalves T, De Ridder L, Driessen A, Lobatón T, Menchén L, Mookhoek A, Noor N, Svrcek M, Villanacci V, Zidar N, Tripathi M. ECCO Topical Review on Clinicopathological Spectrum and Differential Diagnosis of Inflammatory Bowel Disease. J Crohns Colitis. 2022; 16: 343-68.
- Peng C, Zheng C, Xie Y, Sun Q, Zhang X. Granulomatosis with Polyangiitis with colon involvement as a mimicker of Crohn's disease. Clin Res Hepatol Gastroenterol. 2023; 47: 102057.
Presented by
Dr. Johanna Köhler, Linköping, Sweden and Dr. Cord Langner, Graz, Austria.