-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
December 2024
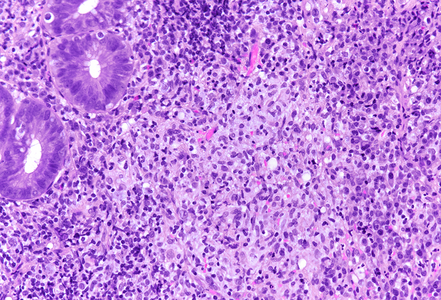
Rectum biopsies from a 35-year-old male with anal pain and haematochezia.
Diagnosis
Chlamydia proctitis (Lymphogranuloma venereum).
Comment
A 35-year-old male having sex with men (MSN) reported about recurrent anal pain, haematochezia and mild diarrhoea. Colonoscopy showed proctitis with edematous and erythematous rectal mucosa and a circumscribed ulcer right above the anal canal. Biopsies were taken. Clinical differential diagnosis: ulcerative proctitis versus infectious proctitis.
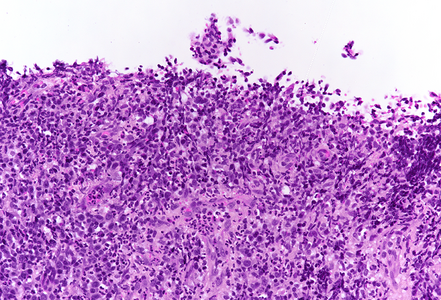
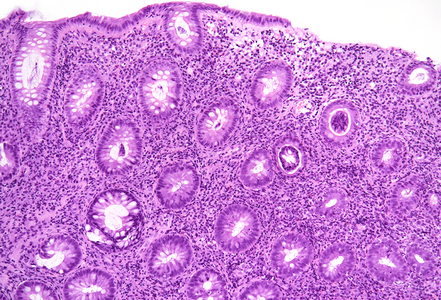
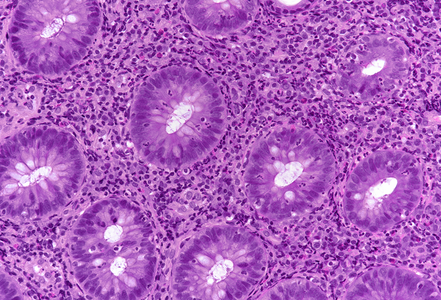
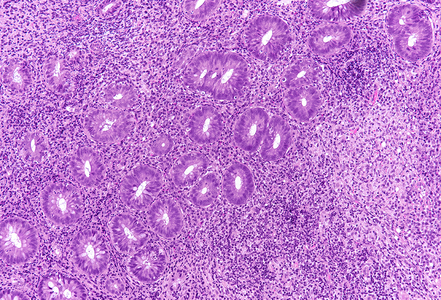
Histological examination disclosed chronically inflamed large bowel mucosa with ulcer and fragments of granulation tissue (Panel A). In the preserved parts of the mucosa, there was mild crypt architectural distortion with occasional branching of crypts, but no prominent crypt irregularities or crypt atrophy (Panel B). The lamina propria contained a dense lymphoplasmacytic infiltrate which extended into the submucosa; few neutrophils and occasional active crypt inflammation / cryptitis were present (Panel C). Deep within the lamina propria an ill-defined non-necrotic granuloma was detected that consisted of a loose collection of epithelioid histiocytes (Panels D-E).
The histological findings were consistent with infectious proctitis, particularly with a sexually transmitted infection (STI). The deep and plasma cell-rich inflammatory infiltrate together with the occurrence of a granuloma indicated Lymphogranuloma Venereum (LGV) which is caused by infection with Chlamydia trachomatis serotypes L1, L2 and L3. Upon request by the clinicians, DNA was extracted from the FFPE biopsy samples and a real-time PCR assay was performed that confirmed presence of Chlamydia trachomatis specific DNA.
STI proctocolitis is underrecognized by clinicians and pathologists due to lacking awareness of the disease and its clinical and histological characteristics. It is often misdiagnosed as inflammatory bowel disease, but there are histopathological features that can help to distinguish STI proctocolitis from IBD. In contrast to IBD, STI proctocolitis is usually lacking prominent crypt architectural distortion, basal plasmacytosis and mucosal eosinophilia. In addition, crypt centered active inflammation (cryptitis, crypt abscesses) is much less pronounced compared to ulcerative proctocolitis and Crohn’s disease. By being familiar with the histopathogical pattern of STI proctocolitis, pathologists can contribute to timely and correct treatment and help to avoid patient mismanagement and STI transmission.
For further reading
- Soni S, Srirajaskanthan R, Lucas SB, Alexander S, Wong T, White JA. Lymphogranuloma venereum proctitis masquerading as inflammatory bowel disease in 12 homosexual men. Aliment Pharmacol Ther. 2010; 32: 59-65.
- Hoentjen F, Rubin DT. Infectious proctitis: when to suspect it is not inflammatory bowel disease. Dig Dis Sci. 2012; 57: 269-73.
- Arnold CA, Limketkai BN, Illei PB, Montgomery E, Voltaggio L. Syphilitic and lymphogranuloma venereum (LGV) proctocolitis: clues to a frequently missed diagnosis. Am J Surg Pathol. 2013; 37: 38-46.
- Arnold CA, Montgomery EA, Voltaggio L. From the pathologist: review of sexual behaviors should be a routine component of clinical histories. Gastrointest Endosc. 2013; 78: 385-6.
- Arnold CA, Roth R, Arsenescu R, Harzman A, Lam-Himlin DM, Limketkai BN, Montgomery EA, Voltaggio L. Sexually transmitted infectious colitis vs inflammatory bowel disease: distinguishing features from a case-controlled study. Am J Clin Pathol. 2015; 144: 771-81.
- Waters KM, Cox BK, Wong MT, Guindi M, Kim SA, Larson BK, Morgan M, Voltaggio L, Balzer BL. Lymphogranuloma venereum (LGV) of the anorectum: evaluation of clinicopathological associations and the utility of a novel RNA in-situ hybridisation stain. Histopathology. 2021; 78: 392-400.
- Ghanta SN, Saccente M. Chronic Lymphogranuloma Venereum Proctocolitis Masquerading as Inflammatory Bowel Disease. J Investig Med High Impact Case Rep. 2022; 10: 23247096221107233.
- Chromy D, Sadoghi B, Gasslitter I, Skocic M, Okoro A, Grabmeier-Pfistershammer K, Willinger B, Weninger W, Öllinger A, Sarcletti M, Stary G, Bauer WM. Asymptomatic lymphogranuloma venereum is commonly found among men who have sex with men in Austria. J Dtsch Dermatol Ges. 2024; 22: 389-97.
- Peuchant O, Laurier-Nadalié C, Albucher L, Balcon C, Dolzy A, Hénin N, Touati A, Bébéar C; Anachla study group.Anorectal lymphogranuloma venereum among men who have sex with men: a 3-year nationwide survey, France, 2020 to 2022. Euro Surveill. 2024; 29: 2300520.
Presented by
Dr. Johanna Köhler, Linköping, Sweden and Dr. Cord Langner, Graz, Austria.