-
Die Universität
- Herzlich willkommen
- Das sind wir
- Medien & PR
-
Studium
- Allgemein
- Studienangebot
- Campusleben
-
Forschung
- Profil
- Infrastruktur
- Kooperationen
- Services
-
Karriere
- Arbeitgeberin Med Uni Graz
- Potenziale
- Arbeitsumfeld
- Offene Stellen
-
Diagnostik
- Patient*innen
- Zuweiser*innen
-
Gesundheitsthemen
- Gesundheitsinfrastruktur
Case of the Month
August 2024
Gastric biopsies from a 68-year-old female with abdominal discomfort.
Diagnosis
Helicobacter pylori gastritis with features of secondary (early) autoimmune gastritis.
Comment
A 68-year-old female underwent gastroscopy, showing mild, unspecific inflammatory changes of the gastric mucosa, and biopsies from antrum and corpus region were taken.
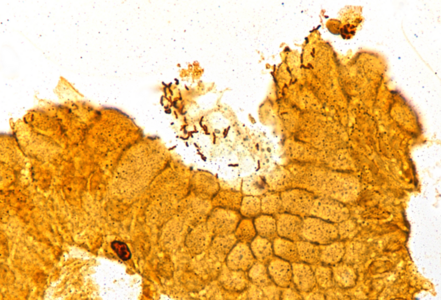
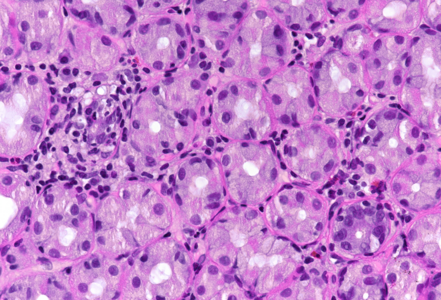
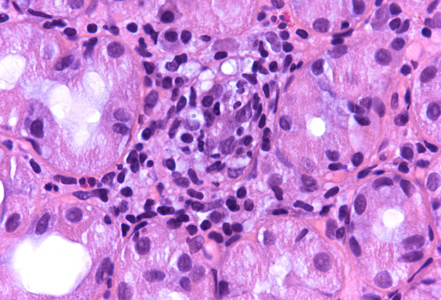
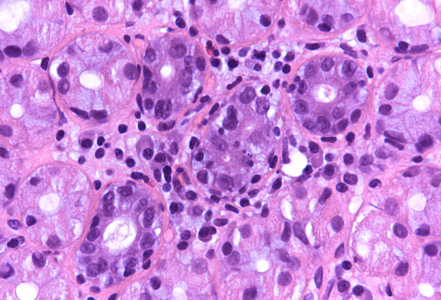
Microscopic examination revealed superficial chronic-active antrum and corpus gastritis (Panel A). In the mucus layer close to the surface epithelium, comma-shaped bacterial structures were detected and highlighted with a Warthin-Starry stain, consistent with Helicobacter pylori (Panel B). In the biopsies obtained from the corpus mucosa, a multifocal, predominantly lymphoplasmacytic infiltrate was seen in deeper parts of the mucosa. Specifically, the oxyntic glands were surrounded and infiltrated by lymphocytes (“emperipolesis”) resulting in gland destruction and parietal cell apoptosis. Occasional eosinophils completed the picture (Panels C-E). No significant atrophy and no metaplastic changes were observed.
Our case is a nice example of Helicobacter pylori gastritis with an anti-gastric component or (secondary) autoimmunity, showing typical features of early autoimmune gastritis, as described by Stolte and co-workers more than 20 years ago. According to the authors, healing of Helicobacter-associated active pre-atrophic autoimmune gastritis by eradication treatment may occur, as indicated in case reports as well as prospective and retrospective studies. Autoimmune gastritis is viewed as the prototype of host-related gastric inflammation. Usually, it develops independently of Helicobacter pylori infection (predominantly in younger or middle-aged females), but may also encounter in usually older patients who are positive for Helicobacter pylori infection. In this setting, antigenic mimicry between bacterial and parietal cell autoantigens may link autoimmune gastritis to previous or current Helicobacter pylori infection (so-called “secondary autoimmune gastritis”).
It is important that pathologists recognize this pattern of secondary (early) autoimmunity in gastritis positive for Helicobacter pylori, as this pattern stresses the need for eradication treatment as well as post-eradication controls. These should be carried out systematically (with biopsies from corpus and fundic region) to follow-up potentially remaining autoimmune gastritis.
For further reading
- Rappel S, Müller H, Stolte M. Die aktive präatrophische Autoimmungastritis Ein praxisorientiertes Konzept für Diagnostik und Therapie. Pathologe 2001; 22: 19–24.
- Veijola LI, Oksanen AM, Sipponen PI, Rautelin HI. Association of autoimmune type atrophic corpus gastritis with Helicobacter pylori infection. W J Gastroenterol. 2010; 16: 83-8.
- Neumann WL, Coss E, Rugge M, Genta RM. Autoimmune atrophic gastritis--pathogenesis, pathology and management. Nat Rev Gastroenterol Hepatol. 2013; 10: 529-41.
- Choudhuri J, Hall S, Castrodad-Rodriguez CA, Westerhoff M, El Jabbour T, Jain S, Panarell NC.; Features That Aid Identification of Autoimmune Gastritis in a Background of Active Helicobacter pylori Infection. Arch Pathol Lab 2021; 145: 1536–43.
- Rugge M, Genta RM, Malfertheiner P, Dinis-Ribeiro M, El-Serag H, Graham DY, Kuipers EJ, Leung WK, Park JY, Rokkas T, Schulz C, El-Omar EM; RE.GA.IN; RE GA IN. RE.GA.IN.: the Real-world Gastritis Initiative-updating the updates. Gut. 2024; 73: 407-41.
Presented by
Dr. Johanna Köhler, Linköping, Sweden and Dr. Cord Langner, Graz, Austria.